Some children who have leukemia or other types of cancer may need a bone marrow transplant (BMT) or a peripheral blood stem cell transplant (PBSCT). In these treatments, the blood cells in the diseased or damaged bone marrow - the spongy material that fills the inside of bones and makes blood cells - are replaced with healthy cells (Stem Cell Transplants), which will grow new healthy cells.
Stem cells are immature cells that produce the three types of blood cells:
- 1. White blood cells, which fight infection.
- 2. Red blood cells, which carry oxygen to and remove waste products from organs and tissues.
- 3. Platelets, which enable the blood to clot.
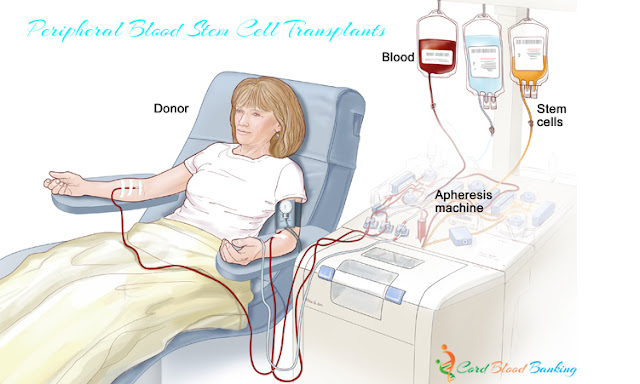
Most stem cells are found in the bone marrow, but some - called peripheral blood stem cells (PBSCs) - are collected from the bloodstream. Umbilical cord blood also contains stem cells. If your doctor proposes a stem cell transplant for your child, the stem cells may come from a donor's bone marrow, bloodstream, or umbilical cord blood or from your child's own bone marrow or bloodstream.
Healthy stem cells grow in two ways:
- . They divide to form more stem cells.
- .They mature into white cells, red cells, and platelets.
Two circumstances create the need for a transplant. The first is when the cancer itself has injured the bone marrow. BMT and PBSCT are commonly used in the treatment of leukemia and lymphoma. The second circumstance is when a treatment requires such large doses of chemotherapy or radiation therapy that the child's bone marrow is damaged during treatment. Chemotherapy and radiation therapy target all cells that divide rapidly. Cancer cells divide more rapidly than most healthy cells and so are destroyed by the therapies. Bone marrow cells, however, also divide more rapidly than other healthy cells, so high-dosage treatment can have a damaging effect on them as well.
A BMT or PBSCT can be done in three ways: as an autologous transplant, an allogeneic transplant, or a syngeneic transplant.
- Autologous transplant - The child's own stem cells or PBSCs cells are used. They can be obtained from the bone marrow or from blood, using the apheresis procedure. Stem cells are collected while the child is in remission. To make sure that any cancer cells that remain are destroyed, the marrow may be treated with anticancer drugs. After the marrow or PBSCs are collected, the child receives high-dose chemotherapy, usually over 2 to 6 days, and, frequently, total body irradiation, during which the whole body is radiated, in one dose or in many doses over several days, to get rid of the cancer. The collected marrow or PBSCs are then returned to the child through a vein, as in a blood transfusion.
- Allogeneic transplant - The marrow or PBSCs from a sibling, parent, or someone not related to the child are used for the transplant. The transplanted material must be as closely matched to the patient's blood cells as possible. Cord blood transplant is allogeneic.
- Syngeneic transplant - The perfectly matched marrow or PBSCs from an identical twin are used for the transplant.
Before the transplant, a catheter is usually inserted into a large vein in the chest for transplanting the marrow or PBSCs, as well as for giving blood, antibiotics, and other drugs and for drawing blood. The child is given high doses of anticancer drugs and/or radiation. When the cancer cells - along with some healthy bone marrow cells - are destroyed, the new, healthy marrow or PBSCs can be given. The healthy marrow or PBSCs are given through the catheter and travel through the bloodstream to the bone marrow where they start to make red and white blood cells and platelets.
It usually takes 14 to 30 days after the transplant for the transplanted stem cells to make enough white blood cells to fight infection and to make other blood cells. During this time, your child will be at higher risk for infections, anemia, and bleeding. Complete recovery of your child's immune system can take 1 to 2 years after an autologous, allogeneic, or syngeneic transplant. Your child may need to remain in a hospital room that is kept as free as possible from anything that may cause an infection. Supportive care, which includes receiving blood transfusions and antibiotics, will be given.
- Supportive Care
Children having a BMT or PBSCT usually stay in the hospital for 1 to 2 months (sometimes longer), although outpatient BMT can be done for children who have brain tumors. Children receiving BMT or PBSCT may need supportive care.
For more information on side effects from chemotherapy and radiation therapy, see the charts in those sections.
- Graft-Versus-Host Disease
The graft-versus-host disease (GVHD) may occur in patients who receive bone marrow or peripheral stem cells from a donor. In GVHD, donated stem cells realize they are in a different body, so they may attack the patient's tissues, such as the liver, skin, or digestive tract. GVHD can be mild or very severe and can occur any time after the transplant - even years later. The doctor may give drugs to reduce the risk of GVHD and to treat the problem if it occurs.
Supportive Care for BMT and PBSCT:
| Problem: | Supportive Care Provided: |
|---|---|
| Low counts of all types of blood cells | Isolation from people with infectious diseases. Transfusion with blood products, including platelets and red blood cells. Treatment with proteins that increase the number of white blood cells. |
| Infections | Intravenous antibiotics. Isolation from other people. |
| Gastrointestinal Infections | Low-bacteria diet. Mouth care. Liquid antibiotics. |
| Difficulty eating enough food | Intravenous nutrition-giving nutrients through a vein. |

No comments:
Post a Comment